gut microbiota
 Gut Microbiota
Gut Microbiota
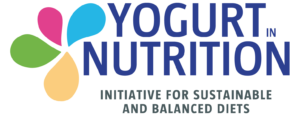
Trillions of bacteria are currently living in our gut in a peaceful relationship with our body. The gut microbiota reveals its secrets little by little. Research found that gut bacteria contribute to keep us healthy. Why is gut microbiota worth of interest?
What is the gut microbiota ?
The gut microbiome or gut microbiota is the ecosystem living in our gut. It is estimated that our gut hosts trillions of microorganisms, which are from about 1000 different species. These microorganisms belong to three domains of life: Microbes, Fungi and Archea. Because of this diversity, these bacteria genes, taken together, add up to more genes than the human host. The set of all microorganisms’ genes is the gut microbiome.
The remarkable feature of this intestinal microbiota is the way it dialogues with our body. Actually, the bacteria genes interact with the human host thanks to cell receptors (located in epithelial, neural or immune cells), hormones and metabolites.
As for now, available evidences have shown that gut microbiota can influence metabolism and the way our metabolism is modified can be beneficial or detrimental, the impact of the microorganisms on gut will depend on their identity and abundance.
There are probably still many things left to discover on the gut microbiota as research only started to explore this subject few years ago. The way gut microbiota influence our metabolism is still under study. However, some data are already available and proven.
How do gut microbiota impact health and diseases?
The spectacular intestinal microbiota living in our body takes part in metabolism in many ways (9). Here are some examples of how the human microbiome impacts health and diseases (10):
- modulation of bone-mass density
- promotion of fat storage
- promotion of angiogenesis
- development and training of the immune system
- biosynthesis of vitamins and amino-acids
- resistance to pathogens
- modification of the nervous system (11)
- modification of appetite regulation
All these examples highlight the tremendous potential of the human intestinal microbiota in both medicine and science. There are probably unknown functions that research will find soon or later.
On the other hand, research suggests that microbial disbalance, or dysbiosis of the gut microbiota could trigger diseases. There is growing evidence that dysbiosis of the gut is linked to pathogenesis of intestinal disorders and extra-intestinal disorders. Intestinal disorders include inflammatory bowel disease, irritable bowel syndrome (IBS) and coeliac disease, whereas extra-intestinal disorders refer to diseases such as cardiovascular diseases, metabolic syndrome, obesity, asthma and allergy.
For instance, some patients suffering from type 2 diabetes have disruptions in the composition and function of their gut microbiota. This observation is in favour of a microbe-mediated development of disease (12).
Could we treat diseases through improving gut microbiota?
Gut microbiota is currently studied for its therapeutic potential in treating obesity and associated metabolic diseases. Indeed, studies have shown that obesity and associated metabolic diseases, such as Type 2 diabetes, are strongly linked with diet. The impact of diet on obesity is commonly agreed. Still, because gut microbiota may reflect both diet and metabolic health, it has become a major topic for research. A body of knowledge presents the gut microbiota as a mediator of dietary impact on the host metabolism.
Gut microbiota are also believed to intervene in our mood and well-being (1). Research reveals that our gut can affect emotional health. Some researchers now focus on understanding how our gut can impact emotional health. This relationship can be modified by the intake of probiotics. Probiotics are believed to shape emotions, sensations and even lower anxiety and depression. This rely on the hypothesis that, through communication between gut microbiota and our brain, probiotics could affect some specific brain activities. When the intestinal barrier is damaged, various neurotransmitters produced by bacteria themselves can cross this barrier and travel to the brain.
How to improve our gut microbiota ?
Lifestyles impact gut microbiota, making it unique for each individual. The three major influence factors having the strongest impact on gut microbiota are:
- nutrition
- environmental exposures to chemicals and drugs
- conditions of birth, which include delivery, feeding, infant care environment but also prenatal events
Besides being unique, gut microbiota evolves through our lifetime. Age, diet, stress, environment, health status, medication exposure (such as the intake of antibiotics) and geography shape our gut microbiota. It is worth mentioning that what we eat may have the greatest impact on gut microbiota and this is something we can pretty much control.
A balanced diet combined with a healthy lifestyle is probably the best way to contribute to gut health, and also to correct dysbiosis. Since food interacts with our microbial tenants, having a look at our eating habits is a way to modulate our microbiota and therefore to improve our health. Dietary patterns and specific nutrients affect significantly the microbial composition.
There is growing evidence that high-fat diets contribute to intestinal dysbiosis, which can lead to a reduced gut permeability. This loss of permeability triggers immune cells which foster inflammation.
Besides, research also underlines the importance of fibers, because low-fiber diets may influence gut microbiota in a way that may have indirectly negative effects on health.
What foods may contribute to the gut health?
We can easily improve our gut health by including some specific foods in our diet. The types of foods that are advisable for taking care of the gut microbiota include:
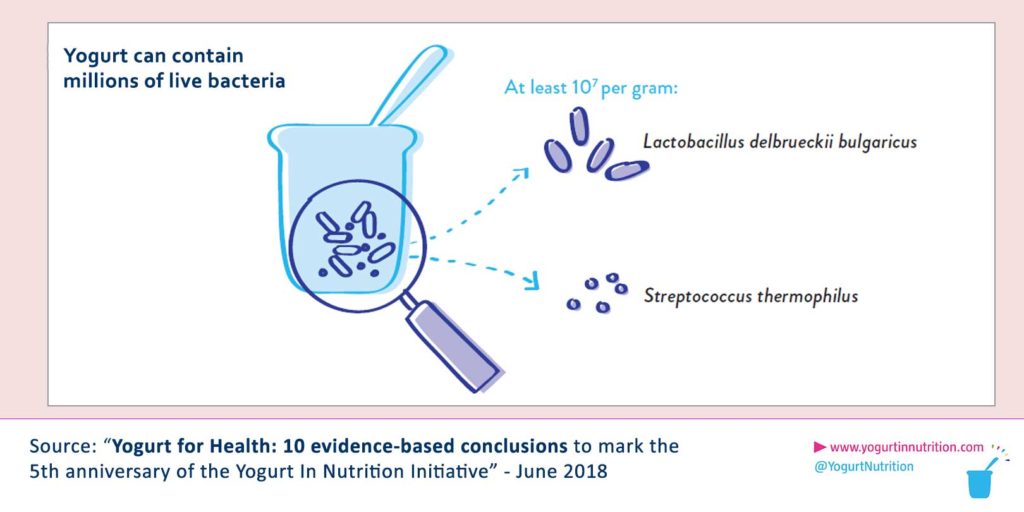
- fermented milk such as yogurt : they deliver many living lactic acid bacteria to the digestive tract. Once they reach the gut, these bacteria sustain the living microbes crossing the gut, at least in a short term. According to researchers, lactic acid bacteria may modulate the intestinal environment, enhance gut permeability and reduce potentially harmful enzymes produced by other bacteria (2).
- fermented foods such as kombucha, kimchi and sauerkraut : they bring replenishment for good gut bacteria (6).
- Dietary fibers rich foods, such as fruits, legumes, vegetables or grains (3).
Because of the growing understanding on how diet, microbiota and health are linked , the intake of both probiotics and prebiotics attract a lot of attention (3).
Can probiotics improve the gut health?
Before answering the question, probiotics and prebiotics shall be distinguished. The World Health Organization (WHO) has defined
- Probiotics as “live microorganisms that, when administered in adequate amounts, confer a health benefit on the host” (you can find probiotics in yogurt for example)
- prebiotics as “selectively fermented ingredients that allow specific changes, both in the composition and/or activity in the gastrointestinal microflora that confers benefits upon host well-being and health”.
More and more studies depict the relationship between probiotics and gut health. The main interest of probiotics is that they provide a way to deliver beneficial bacteria directly to the gut. Medical research is currently evaluating probiotics and prebiotics as potential non-invasive treatments to ease gut disorders (7).
Let’s focus on yogurt and its probiotics. Apart from key nutrients, yogurt also contains living microorganisms, such as Lactobacillus and Bifidobacterium, that positively influence gut disorders (2). The dairy matrix also matters, since it promotes the action of most probiotics. The living organisms of the yogurt alleviate disorders such as IBS, allergic disease, infectious diarrhoea and necrotizing enterocolitis. Then, yogurt consumption has been associated with a better health (4), in particular it has been linked with reduced risks of type 2 diabetes, heart disease, metabolic syndrome and with a better weight management.(8)
Thus, research has proven that preserving the balance of gut microbiota is key to remain in a good health. This is why having a healthy diet is particularly important. Probiotics and fermented foods are under study to determine their potential to positively impact the gut microbiota and to prevent dysbiosis and gut dysfunction (5).
Current research aims at establishing causal relationships between diet, gut microbiota and health (3). It also aims at assessing the possibility to target and modulate gut microbiota for therapeutic interventions.
Sources:
[1] Bienenstock, J. et al., Microbiota and the gut–brain axis , August 2015, Vol 73(8), pp. 28-31.
[2] Hill D, Sugrue I, Arendt E et al. Recent advances in microbial fermentation for dairy and health. F1000Res. 2017;6:751.
[3] Lee Y., Liong M. and Goh K., Probiotics and Prebiotics for gut health: the essentials; WGO Handbook on Diet and the Gut, World Digestive Health Day WDHD – May 29,2016.
[4] Pei Rui-Song (PhD. Nutritional Sciences, University of Connecticut, US), April 2015, Critical Reviews in Food Science and Nutrition
[5] Goulet, O., Potential role of the intestinal microbiota in programming health and disease, Nutrition Reviews, August 2015, Vol 73(8), pp. 32-40.
[6] Tamang JP, Cotter PD, Endo A et al. Fermented foods in a global age: East meets West. Compr Rev Food Sci Food Saf. 2020;19(1):184-217.
[7] Savaiano DA, Hutkins RW. Yogurt, cultured fermented milk, and health: a systematic review. Nutr Rev. 2020 May 23;nuaa013.
[8] Seganfredo FB, Blume CA, Moehlecke M et al. Weight-loss interventions and gut microbiota changes in overweight and obese patients: a systematic review. Obes Rev. 2017 Aug;18(8):832-851.
(9) Bischoff SC. ‘Gut health’: a new objective in medicine?. BMC Med.
2011;9:24.
(10) Pickard JM, Zeng MY, Caruso R, Núñez G. Gut microbiota: Role in
pathogen colonization, immune responses, and inflammatory disease.
Immunol Rev. 2017;279(1):70-89.
(11) de J R De-Paula V, Forlenza AS, Forlenza OV. Relevance of
gut microbiota in cognition, behaviour and Alzheimer’s disease.
Pharmacol Res. 2018;136:29-34.
(12) Hirahatake KM et al Metabolism – Clinical and Experimental Volume 63, Issue 5, Pages 618–627, May 2014