Diabetes
Diabetes : T1D or T2D, GDM
What is diabetes?
Each food intake leads to a rise of carbohydrate (glucose) in the blood, which will be used as energy by the body. This rise of glucose normally triggers the release of insulin. Thanks to insulin, the body cells let glucose come in, and transform it into energy. The level of sugar in blood the glycaemia, is partly regulated by insulin. Once glycaemia goes back to its target value, the blood levels of insulin drop off. Glycaemia must be precisely regulated to remain in its narrow range, so that the body can function optimally.
Diabetes is characterized by an abnormally high glycaemia. When glycaemia chronically outreaches a defined threshold, there is an increased risk of developing adverse long-term effects. These damages and dysfunctions are often related to eyes, nerves, heart, kidney and blood vessels and they are the common symptoms of diabetes.
In the world, about 415 million people have diabetes. By 2040, this number has been estimated to reach 642 million people, which makes it a global health concern.
What are the different types of diabetes?
There are three different types of diabetes:
- Type 1 diabetes or T1D is a form of diabetes where the body does not produce enough insulin. This condition often outbreaks during childhood or adolescence.
- Type 2 diabetes or T2D is a chronic form of diabetes where the insulin produced isn’t efficient enough. T2D whether occurs when the body can’t produce enough insulin or when the body cells become resistant to insulin. Most cases of diabetes are T2D. T2D usually occurs after the age of 45. Nevertheless, the rise of obesity, especially among children, may lead to a rise of T2D which could become a major public issue.
- Gestational diabetes mellitus or GDM is a condition occurring during pregnancy, linked to glucose intolerance and insulin resistant. This condition is usually diagnosed within the second semester of pregnancy. GDM is normally temporary but it is associated with higher long-term risk of developing T2D.
How is diabetes diagnosed?
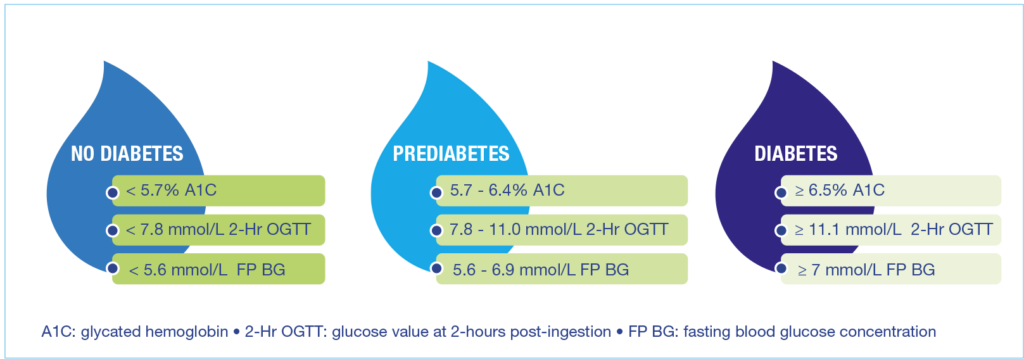
Diabetes and pre-diabetes are usually diagnosed using both the “fasting plasma blood glucose” (FP BG), and the glucose value measured 2 hours after ingestion (2-Hr OGTT). The figure below summarizes the differences between no diabetes, prediabetes and diabetes. When the fasting plasma glucose level is higher than a level that would minimise health risks, it is said that the patient has high blood glucose.
How to distinguish prediabetes and diabetes from no diabetes
What are the treatments for diabetes?
Apart from drugs and insulin injections, given when necessary, lifestyle matters a lot. The World Health Organization (WHO) states that moving to a better lifestyle will both reduce the occurrence of obesity and T2D, and reduce complications for all diabetics. Therefore, the WHO advises people to combine healthy diets, physical activity, and medication if needed, in order to monitor blood glucose level.
For Type 2 diabete (T2D), it is advised to keep an eye on your diet in order to keep from excessive postprandial glycaemic responses (1). And this may be harder than it seems. Indeed, focusing on calories and nutrients is not enough to watch over your diet.
Let’s take the example of proteins. Protein content can lower glycaemic response by increasing insulin secretion. But this effect depends on the source of protein, and insulin is not the only factor involved in glycaemic management.
What is the glycaemic index?
Each food can be characterized by a value called Glycaemic Index (GI). It refers to how fast glycaemia rises after eating a particular food. GI fluctuates between 0 and 100, 100 corresponding to glucose. Food with higher GI will increase blood sugar levels the most. The GI values are divided in three classes:
- “Low GI” gathers foods with GI ≤ 55
- “Medium GI” gathers foods with 55<GI<70
- “High GI” gathers foods with GI≥70
How to select foods regarding the GI?
Because high-GI foods induce a quick spike in blood sugar levels, it is advised, especially for diabetics, not to eat too much food with high GI. Actually, picking low GI meals help people to reduce the GI of their diet.
For example, a plain yogurt is a low GI food (10): the average GI of plain yogurt is 27 (and 41 for sweetened yogurt). The blood sugar response will not be high.
We may also mention that plain and sweetened yogurts have lower GI than what one could expect with its carbohydrate content. Several explanations have been suggested. The lactic acid of the yogurt may slow down gastric emptying and therefore reduce glycaemic response. The amounts of fat, proteins and micronutrients, known to reduce glycaemic response, may also be involved. That is why switching from product with added sugars to yogurt is a healthy choice.
GI is commonly used but there is another value to describe sugar intake. The glycaemic load or GL is calculated with the GI and the amount of carbohydrate of the food consumed.
Can yogurt prevent from T2D risks?
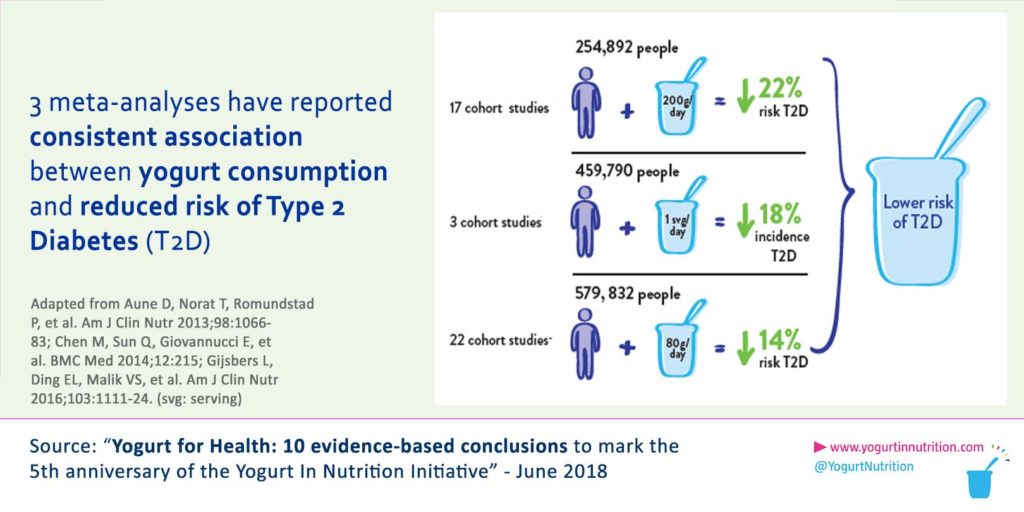
Available data indicate there may be a beneficial association between yogurt consumption and Type 2 diabetes.
A large scale study has also showed that yogurt could help reducing the prevalence of Type 2 diabetes: when the frequency of yogurt consumption increases, the risk of getting T2D declines in a linear relationship (3). Also, as shown in figure 2, yogurt is linked to a healthier insulin profile in children and teenagers.
Several biological mechanisms may explain the benefits of yogurt (2, 3, 4, 7) :
- Yogurt contains live bacteria which, by influencing the gut microbiota, may reduce inflammation. And inflammation is linked to T2D.
- Yogurt consumers are less likely to have unhealthy lifestyles that are linked to T2D.
- Yogurt contains vitamin K2, especially whole-fat yogurt which has up to 28 μg per 100g. The chances of developing T2D decrease by 7% for each extra 10 μg of vitamin K2.
- Yogurt has a low GI (Glycaemic index), and therefore doesn’t lead to a spike in blood glucose after ingestion.
Other studies have shown that yogurt fortified with vitamin D is associated with an improvement in both insulin resistance and lipid metabolism in pregnant women having Gestational diabetes (11). Consuming yogurt supplemented with vitamin D on a daily basis may easily improve GDM (Gestational diabetes mellitus).
Sources:
[1] Wu Y, Ding Y, Tanaka Y, et al. Risk factors contributing to type 2 diabetes and recent advances in the treatment and prevention. Int J Med Sci 2014;11:118–-200.
[2] Chen M, Sun Q, Giovannucci E, et al. Dairy consumption and risk of type 2 diabetes: 3 cohorts of US adults and an updated meta-analysis. BMC Med 2014;12:215.
[3] Aune D, Norat T, Romundstad P, et al. Dairy products and the risk of type 2 diabetes: a systematic review and doseresponse meta-analysis of cohort studies. Am J Clin Nutr 2013;98:1066–83.
[4] Gijsbers L, Ding EL, Malik VS, et al. Consumption of dairy foods and diabetes incidence: a dose-response metaanalysis of observational studies. Am J Clin Nutr 2016;103:1111–24.
[5] Pei R, DiMarco DM, Putt KK, et al. Low-fat yogurt consumption reduces biomarkers of chronic inflammation and inhibits markers of endotoxin exposure in healthy premenopausal women: a randomised controlled trial. Br J Nutr 2017;118:1043–51.
[6] Wen L, Duffy A. Factors influencing the gut microbiota, inflammation, and type 2 diabetes. J Nutr 2017;147:1468S–75S.
[7] Tremblay A, Panahi S. Yogurt consumption as a signature of a healthy diet and lifestyle. J Nutr 2017;147:1476S–80S.
[8] Beulens JW, van der A DL, Grobbee DE, et al. Dietary phylloquinone and menaquinones intakes and risk of type 2 diabetes. Diabetes Care 2010;33:1699–705.
[9] Walther B, Karl JP, Booth SL, et al. Menaquinones, bacteria, and the food supply: the relevance of dairy and fermented food products to vitamin K requirements. Adv Nutr 2013;4:463–73.
[10] Wolever TM. Yogurt is a low-glycemic index food. J Nutr 2017;147:1462S–7S.
[11] Li and Xing, Annals of Nutrition and Metabolism 2016; 68 : 285-290.